What Patients Should Do Immediately After Sample Collection
We’ve all felt that momentary pinch when the needle withdraws after a blood test. While the procedure itself is quick, what you do next matters deeply. Proper steps ensure your body heals smoothly and reduces risks like bruising or swelling.
Within the first hour, keep the protective dressing firmly in place. This simple act gives your body time to form clots and start healing. After 30-60 minutes, you can remove it gently. Avoid tight sleeves or accessories on the arm—opt for loose clothing to let the area breathe.
Strenuous activities? Save them for later. Heavy lifting or intense workouts can strain the needle site, delaying recovery. If you notice slight bleeding, press firmly over the spot with clean fingers for 2-3 minutes. Stay calm—this usually resolves quickly.
Our guide prioritizes your comfort and safety. By following these steps, you take control of your healing journey. Let’s work together to make every blood test experience as smooth as possible.
Guidelines for Immediate Post‑Collection Care
Following blood tests, minor reactions like bruising or tenderness may occur. Our protocols focus on minimizing these effects through proven techniques. Simple actions in the first hour significantly influence recovery speed and comfort.
Proper Dressing and Pressure Application
Keep the initial bandage untouched for 30-60 minutes. This allows clots to form securely. If bleeding resumes, press the area firmly with clean gauze for 2-3 minutes without peeking.
| Step | Action | Duration |
|---|---|---|
| 1 | Maintain initial dressing | 30-60 minutes |
| 2 | Apply direct pressure if needed | 2-3 minutes |
| 3 | Use ice packs for swelling | 10-minute intervals |
Resting and Protecting the Needle Site
Avoid tight sleeves or jewelry on the tested arm. Limit heavy lifting for 4-6 hours. Elevate the arm if discomfort persists, combining rest with cold compresses.
Most patients recover fully within 24 hours. Contact healthcare providers if redness spreads or pain intensifies beyond mild soreness. We prioritize clear communication to ensure safe healing after tests.
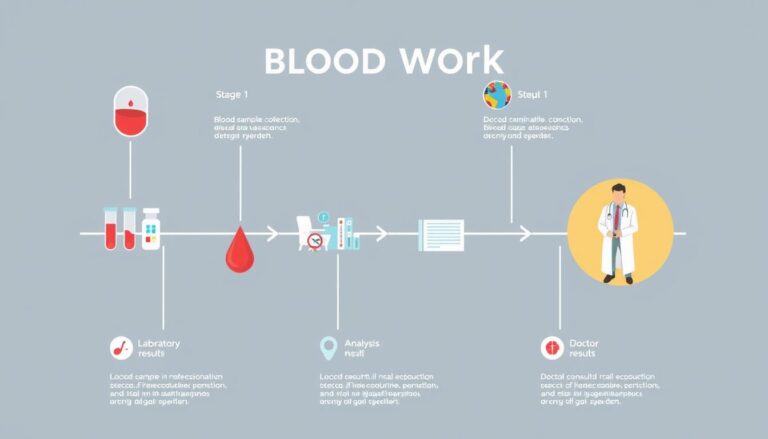
Implementing post‑collection care Protocols for Accurate Test Results
Precision doesn’t end when the needle leaves your arm. Our methods focus on maintaining sample quality while prioritizing your well-being during recovery. These steps directly impact how laboratories analyze your blood and deliver reliable outcomes.

Ensuring Needle Site Integrity and Prevention of Contamination
Clean hands matter when touching the tested area. We advise patients to avoid scratching or pressing the site for 4 hours. Sterile gauze should cover the spot if rebandaging becomes necessary.
Women often require extra vigilance due to vein structure differences. Bruises appear in 14% of cases but fade faster when ice packs are applied early. Those on blood thinners receive customized guidance to minimize swelling.
Managing Discomfort and Recognizing Abnormal Reactions
Dizziness affects fewer than 4% of patients, usually resolving with rest and hydration. Persistent tingling or numbness warrants immediate attention, though such nerve issues remain exceptionally rare.
| Reaction | Frequency | Action |
|---|---|---|
| Bruising | 1 in 7 cases | Cold compress + elevation |
| Fainting | <4% | Lie flat, hydrate |
| Nerve sensitivity | 0.1% | Contact healthcare provider |
We explain how proper aftercare preserves your blood’s condition for testing. Following these steps helps laboratories detect health issues accurately, giving you trustworthy results for informed decisions.
Best Practices for Sample Transportation and Storage
Maintaining sample quality requires precision at every step. From the moment blood leaves the vein to lab analysis, temperature control and handling protocols determine result accuracy. Our systems ensure biological materials stay viable through every phase.

Temperature Control and Safe Packaging
We use medical-grade coolers with temperature trackers for sensitive tests. Blood samples needing IgM/IgG analysis stay at 4-8°C for 24 hours before centrifugation. Serum remains refrigerated up to 7 days, avoiding freeze-thaw cycles that break down proteins.
| Sample Type | Temperature Range | Time Frame | Handling Method |
|---|---|---|---|
| IgM/IgG Blood | 4-8°C | 24 hours | Centrifuge after cooling |
| Serum | 4-8°C | 7 days max | Single freeze cycle |
| Nasopharyngeal | 2-8°C | 48 hours | Triple-layer packaging |
Complying With Labeling Standards
Our phlebotomists label each container with collection dates, patient IDs, and test codes. Color-coded stickers indicate temperature needs. Barcodes sync with digital tracking systems to prevent mix-ups during transportation.
Monitoring Handling Procedures
Couriers complete hourly temperature logs during transit. Shock sensors detect rough handling. Labs verify container integrity upon arrival, rejecting compromised samples immediately. This protects both patients and test results.
Conclusion
Every blood sample’s journey from vein to lab shapes medical decisions. Our methods combine precision handling with patient partnership to protect this vital process. Trained phlebotomists and temperature-controlled systems work together to maintain sample integrity at every stage.
We maintain strict protocols because accurate test results depend on proper conditions. From sterile packaging to real-time tracking, each step prevents contamination. Patients contribute by following after-test guidelines during the critical first hours.
This teamwork ensures laboratories receive viable samples for analysis. Reliable data helps doctors detect health issues early and create effective treatment plans. Our systems evolve using the latest research to improve testing services continually.
Trust forms the foundation of blood testing. When professionals and patients follow proven methods together, we achieve outcomes that transform lives. Your role matters – every action supports health insights that drive better care.